Skin Lesion & Lump Removal in London, ON
Safe, Expert Care for Skin Tags, Moles, Warts, Cysts, Abscesses, and Ganglions
At South London Mole Clinic, we specialize in the assessment and removal of various skin growths and lumps — including skin tags, moles, warts, cysts, abscesses, and ganglions. Our expert team led by experienced Nurse Practitioners uses advanced techniques to ensure safe, effective, and comfortable treatments tailored to your unique needs.
Located conveniently in
London, Ontario.
Book your
Book your Mole removal consultation today.
South London Mole Clinic

We offer several safe and effective removal techniques for skin tags and moles. Our treatments are performed by experienced Nurse Practitioner using modern medical equipment and techniques.
Our Nurse Practitioner will thoroughly assess your specific case and recommend the most appropriate removal method during your consultation.
Available
Removal Methods:
Cryotherapy for Moles, Skin Tags & Warts
Cryotherapy is a precise, controlled freezing technique that is suitable for smaller skin tags and certain types of moles, offering a quick procedure with minimal discomfort.
What is cryotherapy?
Cryotherapy uses liquid nitrogen or a cooled spray to freeze abnormal tissue. Freezing causes the treated tissue to break down over days to weeks and fall away, allowing healthy skin to regenerate. It is a rapid, widely used method for treating warts, skin tags, and other superficial benign lesions.
Conditions commonly treated
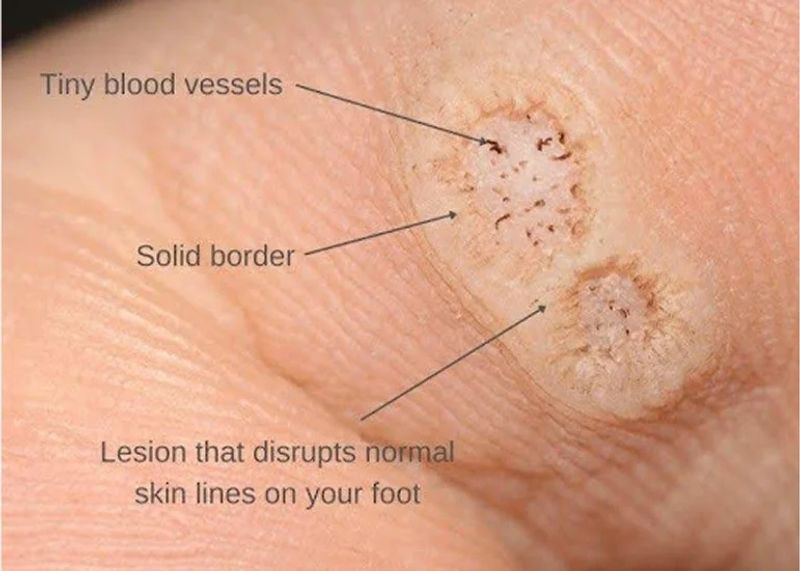
- Common viral warts (hands, feet, body)
- Skin tags (small benign skin growths often in skin folds)
- Certain benign-appearing moles (only after clinical assessment — suspicious or atypical lesions will be prioritized for biopsy or alternative management)
- Actinic keratoses and other superficial lesions where appropriate
Important: we do not perform cryotherapy on lesions that look suspicious for melanoma or other skin cancers. Any lesion with concerning features will be assessed and managed accordingly.
What to expect during the appointment
- Assessment: A clinician reviews your medical history and examines the lesion(s) to confirm cryotherapy is suitable.
- Consent & explanation: We explain the procedure, expected outcomes, and possible side effects.
- Treatment: The lesion is frozen briefly using liquid nitrogen delivered by spray or probe. Treatment time varies depending on size and location.
- Aftercare: The treated area may blister or scab; we provide clear instructions for wound care, signs of infection, and follow-up.
Cryotherapy is usually quick (a few minutes). Multiple sessions may be required for some warts.
Benefits and possible side effects
Benefits: Quick in-office treatment, minimal downtime, effective for many benign lesions.
Possible side effects: Temporary pain, blistering, scabbing, pigment change (lightening or darkening of the skin), scarring (rare). Our clinicians take care to minimize these risks.
Who performs the treatment?
Treatments are performed by our experienced and professional medical staff — including Nurse Practitioners and/or physicians trained in dermatologic procedures. We adhere to strict standards for safety, infection control, and documentation.
Is cryotherapy right for me?
Cryotherapy is a great option for many superficial benign lesions, but it may not be suitable in all cases. You should consult our team if your lesion is rapidly growing, painful, bleeding, or changing in colour or shape — such features may require biopsy or referral to dermatology.
Pricing & insurance
Pricing depends on the number and size of lesions treated. We provide an estimate during your assessment. Receipts can be provided for private insurance where applicable.
Book an assessment
To arrange an assessment with our medical team, please call or email. We’ll review your concern and advise whether cryotherapy is the recommended option, or if further evaluation is needed.
Shave Excision for Moles, Skin Tags & Warts
Shave Removal is a gentle procedure that removes growths at skin level, making it ideal for raised lesions and typically resulting in minimal scarring.
To book:
What is shave excision?
Shave excision removes a raised lesion by shaving it off parallel to the skin surface after local anaesthesia. It is best suited for lesions that are elevated above the skin and benign in appearance. The procedure is quick and typically performed in-clinic with minimal downtime.
Suitable lesions
- Raised benign moles (selected cases following clinical assessment)
- Skin tags (particularly small to medium-sized tags)
- Superficial warts and verrucae
- Certain benign keratoses and cosmetic raised lesions
If a lesion looks suspicious for melanoma or other skin cancer, shave excision may not be appropriate — such lesions will be prioritised for full excision or biopsy and specialist referral if needed.
Procedure overview
- Assessment: A clinician reviews your history and examines the lesion to confirm suitability.
- Local anaesthetic: The area is numbed to minimise discomfort.
- Shave excision: The clinician removes the raised portion with a sterile blade or curette; bleeding is controlled with cautery or pressure.
- Specimen handling: If clinically indicated, the removed tissue may be sent for histopathological (laboratory) examination to ensure there are no unexpected or atypical cells.
- Aftercare & follow-up: The wound is dressed and you receive clear instructions. We arrange follow-up to check healing or discuss pathology results if a specimen was sent.
Most shave excisions are completed within a single visit. Sending a sample for histopathology is done when there is any clinical reason to evaluate the tissue under the microscope — this is an important safety step when appropriate.
Benefits & risks
Benefits: Rapid procedure, minimal downtime, often good cosmetic outcome for raised lesions, and the ability to send tissue for histopathology when indicated.
Risks: Bleeding, infection, pigment changes (hypo- or hyperpigmentation), scarring, and the possibility of incomplete removal requiring further treatment. Rarely, pathology may reveal unexpected findings which we manage promptly.
Histopathology — when and why
Our clinician may decide to send the excised tissue for histopathological examination if there are any atypical features, uncertainty about the diagnosis, patient preference, or as a routine precaution for certain lesions. Histopathology provides a definitive microscopic diagnosis and helps rule out malignancy. We will discuss this option and any associated costs during your consultation.
Who performs shave excision?
Shave excisions are performed by our experienced medical staff — Nurse Practitioners trained in minor surgical dermatologic procedures. We follow strict clinical and infection-control standards and prioritise your comfort and cosmetic outcome.
Is shave excision right for me?
Suitability depends on lesion type, size, location and your medical history. Book an assessment so our clinicians can recommend the optimal approach — whether shave excision, full-thickness excision, cryotherapy, or biopsy.
Costs & insurance
Costs depend on lesion complexity, whether histopathology is requested, and the number of lesions treated. We will provide an estimate at consultation. Receipts are available for private insurance claims.
Book an assessment
To schedule an appointment or ask questions, call or email our clinic. We will assess your lesion, discuss the likely outcome, and advise if sending tissue for histopathology is recommended.
Elliptical Excision for Moles & Cysts
Elliptical Excision is a complete surgical removal procedure recommended for deeper moles or suspicious lesions, allowing for pathological examination if required.
Book an appointment:
What is elliptical excision?
Elliptical excision (also called an ellipse or full-thickness excision) involves removing a lesion with an elliptical incision that includes the full thickness of the skin. This approach allows complete removal of the lesion and tight, neat closure of the wound in layers to optimise healing and cosmetic outcome.
When is it recommended?
- Moles that are suspicious, changing, or where complete removal is desired for diagnosis.
- Cysts that require full excision to remove the entire cyst sac and reduce recurrence.
- Lesions in areas where a stronger closure is required for cosmetic or functional reasons.
The clinician will assess each lesion to determine the most appropriate technique — occasionally smaller or less invasive treatments may be recommended instead.
Procedure — step by step
- Consultation & consent: Review of your medical history, examination of the lesion, and discussion of options including risks, benefits and expected scar.
- Local anaesthetic: The area is numbed to ensure you are comfortable during the procedure.
- Elliptical excision: The clinician marks an elliptical shape around the lesion, removes the lesion full-thickness, and if necessary, removes adjacent tissue to achieve clear margins.
- Layered closure: The wound is closed in layers with fine sutures to reduce tension on the skin and improve cosmetic outcome. External sutures are usually removed after an interval depending on location.
- Specimen handling: When clinically indicated, the excised tissue is sent for histopathological examination to confirm the diagnosis and ensure margins are clear.
- Aftercare & follow-up: We provide wound-care instructions and schedule follow-up for suture removal and to review pathology if a specimen was sent.
Benefits & potential risks
Benefits: Complete removal with reduced risk of recurrence (especially for cysts), ability to obtain a definitive diagnosis via histopathology, and controlled cosmetic closure.
Risks: Bleeding, infection, scarring, numbness around the surgical site, and—rarely—poor wound healing. The clinician will explain specific risks based on lesion location and your medical history.
Histopathology — important safety step
When there is any clinical concern, uncertainty about diagnosis, or whenever a definitive diagnosis is desired, the removed specimen will be sent to a pathology laboratory. Histopathological examination provides a microscopic diagnosis and confirms whether complete excision was achieved. We will inform you of results and any further recommendations.
Who performs elliptical excisions?
Elliptical excisions are performed by our experienced medical staff — Nurse Practitioners trained in minor surgical procedures. We follow strict sterile technique and surgical principles to ensure safety and optimal outcomes.
Is elliptical excision right for me?
Suitability depends on lesion type, size, location and your medical history. Book an assessment and our clinicians will recommend the safest, most effective option — which may include elliptical excision, shave excision, cryotherapy, or referral for specialist care.
Costs & insurance
Costs depend on lesion complexity, requirement for histopathology, and the number of lesions treated. We provide an estimate at consultation. Receipts for private insurance claims are available upon request.
Book an assessment
To arrange a consultation or to ask questions, call or email our clinic. We will assess your lesion, discuss the likely procedure and scarring, and advise whether histopathology is recommended.
Pre- & post-operative guidance
Electrocautery (Cauterization) for Skin Lesions
Cauterization is a controlled heat treatment used to remove growths, effectively targeting small to medium-sized lesions with precision.
To book:
Common lesions that can be treated with electrocautery
Electrocautery is commonly used for selected benign lesions including (but not limited to):
- Skin tags (acrochordon)
- Dermatosis papulosa nigra (DPN)
- Cherry angiomas (senile angiomas)
- Small haemangiomas and angiokeratomas
- Viral warts (common and plane warts — selected cases)
- Superficial seborrhoeic / seborrheic keratoses (in selected cases)
- Milia and small epidermal inclusion cyst openings
- Pyogenic granuloma (careful assessment required)
- Telangiectasia / small superficial blood vessels (selected cases)
- Certain benign horny lesions and small benign papillomas
Not all lesions are suitable for electrocautery. Lesions that are suspicious for skin cancer or have atypical features should not be treated with cautery — they require excision or biopsy so tissue can be examined under the microscope.
Assessment — safety first
Before any procedure our clinician conducts a thorough assessment. If there is any doubt about the diagnosis or concerning features (irregular border, rapid change, bleeding, varied colour, or large size), we will recommend excisional biopsy or referral rather than destroying tissue with cautery. This ensures suspicious lesions can be sent for histopathology and receive appropriate care.
How the procedure works
- Consultation: Review of medical history and lesion examination.
- Local anaesthetic (if needed): For comfort, the area may be numbed with local anaesthetic depending on lesion size and location.
- Cauterization: The clinician uses an electrocautery device to remove or coagulate the lesion. Treatment time is short — often a few seconds to a few minutes per lesion.
- Wound care: The treated area may crust or scab; we provide aftercare instructions and advice on signs of infection.
- Follow-up: We arrange follow-up as needed; if a biopsy or excision is required instead, we will explain next steps.
Because electrocautery destroys tissue, it generally does not yield a specimen suitable for histopathology. That is why careful clinical assessment is essential before choosing this method.
Benefits & possible side effects
Benefits: Fast in-office treatment, minimal equipment, often excellent results for small benign lesions, and low downtime.
Possible side effects: Local pain, blistering, crusting, temporary or permanent pigment change (hypo- or hyperpigmentation), scarring (rare), and infection. Our clinicians use precise technique to minimise these risks.
When histopathology is needed
If any lesion has suspicious features or if a definitive diagnosis is required, our clinician will recommend excisional biopsy (which provides tissue for histopathology) rather than cautery. This is an important safety step — electrocautery destroys tissue and prevents later microscopic analysis.
Who performs electrocautery?
Treatments are performed by experienced and professional medical staff — Nurse Practitioners trained in minor surgical and electrosurgical techniques. We follow strict infection-control standards and clinical guidelines.
Pricing & booking
Costs vary by lesion number, size and complexity. We provide an estimate at assessment. Receipts are provided for private insurance claims where applicable.
Punch Biopsy for Skin Lesions
South London Mole Clinic – London, Ontario
Educational Information About Punch Biopsy & Its Role in Skin Health
A punch biopsy is a procedure where a small, tube-shaped piece of skin and underlying tissue is removed using a sharp, circular cutting tool, and the tissue is then examined under a microscope to check for signs of disease.
Understanding Punch Biopsy
A punch biopsy is a commonly used dermatological procedure designed to obtain a small, full‑thickness sample of skin for diagnostic evaluation. It allows clinicians to examine the skin at a microscopic level to better understand a lesion’s nature—whether benign, inflammatory, infectious, or potentially cancerous.
This page is intended to help patients learn what a punch biopsy is, when it may be recommended, and why histopathological examination is important.
Why Punch Biopsy Is Performed
Punch biopsy is used when visual inspection alone cannot provide a definitive diagnosis. It helps clarify:
- The cause of a changing or atypical mole
- Suspicious skin lesions that may require further evaluation
- Rash or inflammatory skin conditions
- Skin infections with uncertain appearance
- For complete removal of benign, non- cancerous mole
A clinician will recommend a punch biopsy only when it is medically appropriate, based on the lesion’s appearance, symptoms, and any changes over time.
Common Skin Lesions That May Require Punch Biopsy
Punch biopsy may be indicated for a wide range of lesions and conditions.
Pigmented Lesions / Possible Skin Cancers
- Atypical or irregular moles
- Changing moles or new pigmented lesions
- Lesions that may represent melanoma, basal cell carcinoma (BCC), or squamous cell carcinoma (SCC)
Benign Lesions When Diagnosis Is Uncertain
- Dermatofibromas
- Seborrheic keratoses with unusual features
- Angiofibromas
- Lipomas (to confirm diagnosis when necessary)
- Epidermoid/epidermal inclusion cysts
- Benign adnexal tumors
Inflammatory or Autoimmune Skin Conditions
A punch biopsy can help confirm:
- Eczema variants
- Psoriasis
- Lichen planus
- Cutaneous lupus
- Granulomatous diseases
- Vasculitis
- Drug-related skin reactions
- Autoimmune blistering disorders
Infectious Lesions (when diagnosis cannot be made clinically)
- Uncertain fungal, bacterial, or viral skin infections
Not every lesion requires a biopsy—your clinician will assess whether this technique is necessary based on clinical criteria.
Histopathology: Why It Matters
Punch biopsy samples are almost always sent for histopathological examination, where a medical laboratory analyzes the tissue under a microscope.
Histopathology helps:
- Confirm benign vs. malignant features
- Identify early skin cancers
- Provide clarity for persistent rashes
- Guide correct treatment plans
This detailed analysis is a key part of safe, evidence‑based skin care.
What the Procedure Typically Involves
A punch biopsy is generally a quick procedure performed under local anesthesia. It involves:
- Cleaning the area
- Injecting a small amount of anesthetic
- Using a circular tool to remove a tiny skin sample
- Placing a suture when necessary
- Applying a small dressing
Most patients experience minimal discomfort, and healing is usually straightforward.
Aftercare & Healing
- Mild tenderness for a day or two is normal
- The area should be kept clean and protected
- Sutures (if used) are usually removed within 7–10 days
- Patients are advised to avoid friction and stretching of the area
Your clinician provides individualized aftercare instructions to ensure proper healing.
A Patient‑Centred Approach
At South London Mole Clinic, punch biopsy is used only when clinically indicated. Our goal is to ensure:
- Accurate diagnosis
- Evidence‑based decision‑making
- Patient comfort and understanding
- Early detection of conditions that benefit from timely care
This page is for educational purposes to support informed discussions during your consultation.
Questions?
If you have concerns about a mole or skin lesion, discuss them with your clinician, who can determine whether a punch biopsy—or a different diagnostic method—is the most appropriate next step.
Incision and drainage (I&D), also known as clinical lancing, is a minor surgical procedure to release pus or pressure buildup under the skin, typically from an abscess, boil, or infected paranasal sinus, by making an incision and draining the fluid.
Nd Yag lasers emit specific wavelengths of light that are preferentially absorbed by melanin, the pigment responsible for skin color. This absorbed energy transforms into heat, effectively destroying the melanin-rich cells without affecting the natural skin color.
Swift® Laser Wart Treatment
South London Mole Clinic – London, Ontario
Advanced Technology • Immune-Based Therapy • Dual‑Action Approach
Swift therapy utilizes microwave energy to penetrate the skin and heat the wart tissue to a precise temperature, effectively destroying the wart while minimizing harm to surrounding healthy skin.
Swift® Laser Wart Treatment
At South London Mole Clinic, we offer Swift® microwave therapy, an advanced non-invasive treatment designed to target the underlying cause of warts—the virus itself. Swift therapy works by delivering a precise dose of microwave energy into the wart, stimulating a powerful immune response from within.
To enhance results, we pair Swift treatment with complimentary cryotherapy during the same session when clinically appropriate. This combination provides a dual‑action approach:
- Swift® Laser (Microwave Energy): Initiates an internal immune reaction to clear the viral infection.
- Cryotherapy: Creates a controlled frostbite effect externally to disrupt the wart tissue.
Together, these two mechanisms support a more effective eradication of stubborn and long‑standing warts.
How Swift® Therapy Works
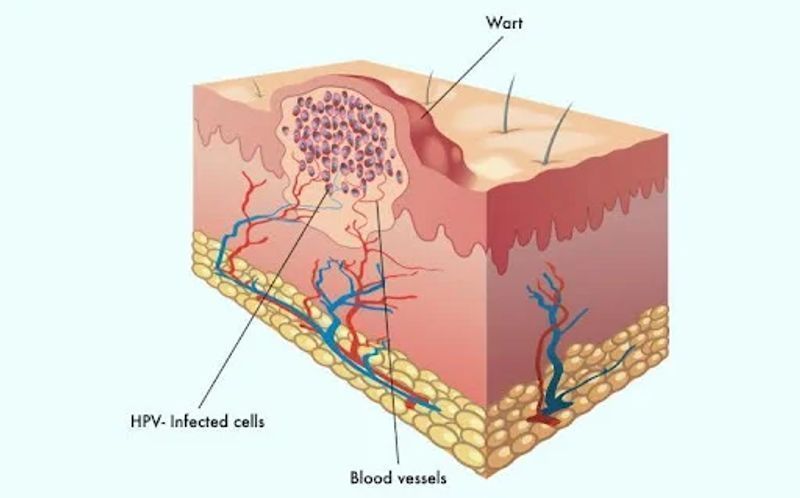
Swift® uses a specialized microwave handpiece to deliver short, targeted energy pulses to the wart. This energy doesn’t damage the skin—they instead activate the body’s immune system, encouraging it to recognize and fight the underlying human papillomavirus (HPV).
Benefits of Swift® Wart Treatment:
- Safe and non-invasive
- No cutting or injections
- Minimal discomfort
- Treatment sessions are quick (just a few seconds of energy delivery)
- No dressings, downtime, or wound care needed
- Stimulates long-lasting immune protection
Dual‑Action Therapy: Swift® + Cryotherapy
Because warts can be persistent and deeply rooted, our clinic offers cryotherapy as a complimentary add‑on to Swift® treatment.
Why Combine the Two?
- Swift® triggers an immune response from the inside, helping the body identify and clear the virus.
- Cryotherapy damages the outer wart tissue from the outside, promoting shedding and disrupting viral cells.
This dual‑action approach can be especially valuable for:
- Long‑standing warts
- Warts that failed other treatments
- Plantar warts causing discomfort
- Clustered or mosaic warts
- Immune‑resistant cases
When Swift® May Not Be Appropriate
While Swift® is suitable for many patients, it is not recommended in certain cases—for example:
- Patients with implanted electronic devices (e.g., pacemakers) without prior clearance
- Metal plates or pins near the treatment area
- Pregnant individuals (as a precaution)
- Certain medical conditions affecting sensation or healing
If Swift® is not appropriate, we will recommend a suitable alternative, such as:
- Cryotherapy alone
- Electrocautery
- Shave removal
- Chemical treatments (as medically indicated)
- Watchful waiting for non-problematic lesions
Your clinician will always guide you toward the safest and most effective treatment option.
What to Expect During a Swift® Session
- The lesion is assessed to confirm its suitability for Swift® therapy.
- Short bursts of microwave energy are delivered to the wart (usually 2–5 seconds each).
- Cryotherapy may be applied immediately after to reinforce treatment.
- No dressings are required—normal activities can be resumed right away.
- Multiple sessions are often recommended, spaced 2–4 weeks apart.
Frequently Asked Questions
Is Swift® painful?
Most patients describe the sensation as a brief, sharp heat lasting only a few seconds.
How many treatments will I need?
Typically 3–4 sessions, though resistant or long‑standing warts may require additional treatments.
Does Swift® leave scars?
No—Swift® does not break the skin and does not require healing time.
Why do warts need immune‑based therapy?
Warts persist because the immune system often fails to detect the infection. Swift® helps the body recognize and clear the virus naturally.
An Evidence-Based, Patient-Focused Approach
Our medical team is trained and experienced in providing advanced wart care. We believe in combining the latest technology with clinical expertise to ensure safe, effective treatment tailored to your needs.
Interested in Learning More?
If you’re dealing with a stubborn wart or have questions about Swift® laser therapy, our team is here to help.
Phone: 519-800-4518
Email:info@southlondonmoleclinic.ca
Location: South London Mole Clinic, 561 Southdale Road East, Unit 10, London, Ontario
This page is for informational purposes only and does not replace professional medical advice. All treatments are offered based on clinical assessment and suitability.
Intralesional Steroid (Kenalog®) Treatment
South London Mole Clinic – London, Ontario
Educational Information About Steroid Injections for Keloids & Cystic Acne
Kenalog (triamcinolone acetonide) injections are a common and often effective treatment for keloid scars, working by reducing inflammation and breaking down excess collagen to flatten and soften the scar tissue.
Understanding Intralesional Steroid Injections
Intralesional steroid injections—most commonly using Kenalog® (triamcinolone acetonide)—are a well‑established medical treatment for certain skin conditions that benefit from targeted reduction of inflammation, thickening, or scar tissue.
At South London Mole Clinic, this treatment is offered by experienced medical professionals when clinically appropriate. This page provides educational information about how Kenalog® injections work, when they may be recommended, and what alternatives may be considered.
What Is Kenalog® (Triamcinolone Acetonide)?
Kenalog® is a corticosteroid that reduces inflammation and excessive collagen production within the skin. When injected directly into a lesion, it can help flatten, soften, or calm areas of overgrowth or inflammation.
This treatment is localized—meaning the steroid acts mainly where it is injected, minimizing effects elsewhere in the body.
Conditions Commonly Treated With Intralesional Steroid Injections
Kenalog® may be used when clinically appropriate for:
Keloids & Hypertrophic Scars
- Raised, firm, or itchy scars
- Keloids that continue growing beyond the original injury
- Thick scars that interfere with comfort or appearance
Cystic or Nodular Acne Lesions
- Deep, painful acne cysts
- Nodular inflammatory lesions
- Breakouts at risk of scarring
Other Dermatologic Conditions (case‑by‑case assessment)
- Localized inflammatory nodules
- Certain benign growths requiring inflammation control
- Granulomatous lesions
Not all lesions are appropriate for steroid injection—a medical assessment is always necessary.
How Intralesional Kenalog® Works
When injected into a targeted area, Kenalog®:
- Reduces inflammation
- Decreases thickened scar tissue
- Slows collagen overproduction (helpful for keloids)
- Shrinks painful acne cysts
- Speeds resolution while lowering risk of scarring
The dosage and concentration are carefully chosen based on lesion type, size, and body area.
When Kenalog® May Not Be Appropriate
There are situations where steroid injections may not be the preferred or safest option, such as:
- Thin or delicate skin areas (risk of atrophy)
- Very large keloids requiring surgical or combination therapy
- Active infection at the site
- Certain medical conditions or medications
- Repeated injections in the same area
In these circumstances, alternative treatments may be recommended, including:
- Silicone gel or silicone sheeting
- Cryotherapy for keloids
- Surgical excision (with or without adjunct therapies)
- Acne treatment plans (topical, oral, or procedural)
- Laser therapy for scars or redness
- Drainage of acne cysts when necessary
Your clinician will help determine the safest, most effective path based on individual evaluation.
What to Expect During Treatment
An intralesional injection is generally quick and well‑tolerated:
- The area is cleansed.
- A very small needle delivers a measured dose of steroid directly into the lesion.
- Discomfort is typically minimal and brief.
- Improvement may be noticeable within a few days (for acne) or over several weeks (for keloids).
Multiple sessions may be suggested for thicker keloids or recurring inflammation.
Potential Side Effects
Side effects are usually mild but may include:
- Temporary skin lightening (hypopigmentation)
- Skin thinning or small depressions at the injection site
- Redness or tenderness
- Delayed response requiring additional treatments
Your clinician will discuss risks and benefits prior to proceeding.
A Balanced, Evidence‑Based Approach
At South London Mole Clinic, intralesional steroid injections are used only when medically indicated and tailored to each patient’s needs. The goal is to:
- Support healing
- Reduce discomfort
- Minimize scarring
- Provide safe, research‑based care
This information is intended to support your understanding and help guide conversations during your consultation.
Questions?
If you are unsure whether a keloid, scar, or inflammatory lesion requires treatment, a clinician can help determine the most suitable approach—including whether Kenalog® is appropriate or if an alternative is recommended.
Location: South London Mole Clinic, 561 Southdale Road East, London, Ontario
This page is for educational purposes only and is not a substitute for medical assessment or individualized advice.
Gallery
Areas Treated with
Skin Tags, Moles, Warts, Cysts, Abscess, and Ganglion Removal
Testimonials
What Our Patients Say
Testimonials